H. Pylori (Helicobacter pylori) – is a helix-shaped (classified as a curved rod, not spirochaete) Gram-negative bacterium that colonizes the gastric mucous layer. Infections of H. Pylori are usually acquired in early childhood in all countries either due to inadequate hygiene education or parent-to-child contact. If a person is infected and becomes compromised due to stress, an illness or a poor diet, left untreated, presence of H. Pylori dramatically increases risks for digestive and systemic ailments.
H. pylori is contagious. It is estimated that over 70% of population infected with the bacterium and 10%-15% of those infected experience symptoms of H. Pylori overgrowth.
The following routes of transmission are likely to be most frequently occurring
- Food and water contamination (primary causes)
- Eating utensils and drinking cups contamination at home and restaurants
- Public restroom faucets and door knobs contamination
- Oral-to-oral contact
- Dental office instruments
In many people H. Pylori does not cause significant symptoms as its growth is controlled by the immune system, healthy intestinal flora, capacity of glutathione and acidity of the stomach. A copper deficiency may contribute to susceptibility to H.Pylori overgrowth due to impaired white blood cells proliferation.
Since the infection affects the parietal cells that produce stomach acid [srs], anyone who has the infection, becomes more susceptible to digestive ailments. Combined with an unhealthy diet and usage of stomach acid reducers, a vicious cycle can be triggered. Invasion and multiplication of H. Pylori deeper into the tissues can progressively worsen the health of parietal cells further reducing the protective mechanism of gastric acid. Consequently, a further implication of opportunistic pathogens eventually may results in adverse health conditions on a systemic level.
H. Pylori induced conditions
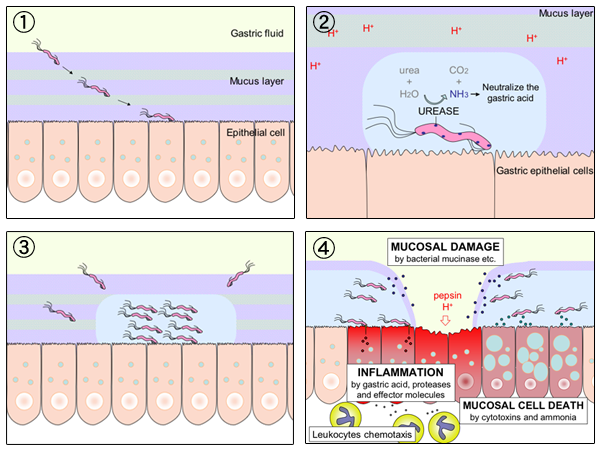
The infection suppresses the stomach acid secretions by producing a urease enzyme that catalyzes hydrolysis of urea into carbon dioxide and ammonia. The ammonia in turn is toxic to epithelial cells that produce gastric acid. [srs]
The following is the mechanism by which H.Pylori induces gastric ulcers and reduces the gastric acid production
- The bacterium penetrates the mucus layer of stomach and mounts onto the surface of gastric mucosal epithelial cells. It then produces ammonia from urea.
- The ammonia secretion protects H. Pylori by neutralizing gastric acid allowing the bacterium to further replicate and further infect the surrounding tissues.
- Gastric ulcers arise from destruction of mucosa, inflammation and mucosal cell death.
- When ulcers appear, the affected individuals usually rely on acid suppression medications, further allowing the bacterium to spread and deactivate epithelial cells that produce gastric acid.
By Y_tambe (Y_tambe’s file) [GFDL
More than 90% of duodenal ulcers and up to 80% of gastric ulcers are caused by H. Pylori. The infection is also a factor in possible initiation of autoimmune complexes [srs].
Symptoms and facts about H. Pylori induced conditions
- Hypochlorhydria (decreased stomach acidity)
- Indigestion, acid reflux, GERD, stomach pain and constipation
- Depletion of antioxidant glutathione due to increased oxidative stress [srs]
- Abnormally yellow/pale stools
- Brain fog due to ammonia toxicity
- Burping and gas immediately after eating
- Fungal overgrowth due to dysbiosis
- Dermatitis, rosacea
- Bowel hyper permeability / Leaky gut
- Food and environmental allergies due to H. Pylori induced mast cells degranulation [srs]
- Decrease in conversion of T4 to Active T3 thyroid hormones. When metabolic stress is created, T3 converts to RT3 (reversed T3) causing symptoms similar to hypothyroid such as fatigue, dry skin, depression, weight gain and insomnia
- Decrease in iron absorption [srs]
- Atrial fibrillation
- Abnormal lipid and CRP levels. Treating the infection may normalize cholesterol HDL levels and decrease CRP levels [srs]
- Halitosis (bad breath) and periodontal disease
- Sustained metabolic stress on the body detoxification pathways affecting the liver, pancreas and kidney functions
- 1–2% lifetime risk of stomach cancer by inducing production of free radicals and an increased host cell mutation
- Autoimmune inflammatory conditions caused by mineral deficiencies and pathogenic bacteria and fungus overgrowth. These may include but not limited to Addison’s disease, CFS, FMS, asthma, systemic lupus, erythematosis
- Adrenal fatigue due to overstimulation by increased ammonia concentration in brain
- Osteoporosis
- Sjogren’s syndrome
- Raynaud’s syndrome
- Gastric carcinoma and lymphoma
- Fibromyalgia implications
- Coronary heart disease
- Induced vitamin D and manganese deficiency
- Niacin deficiency (mainly due to deficiency of tryptophan)
Testing
The most reliable and the least invasive way of testing is stool antigen. The stool culture can remain positive 2-3 months after treatment, therefore retesting is warranted 2-3 months post treatment. A blood antibody test will remain positive after eradication, indefinitely. Carbon urea breath test is an alternative method of testing that has a very little latency after the treatment but not as sensitive as a stool culture test.
However, biopsy during an endoscopy with a rapid urease test, histological examination, and microbial culture is the most reliable but an invasive method of testing for H. Pylori infection. It is warranted if the symptoms persist without positive identification on blood, stool and breath tests. Additionally, a urine ELISA test with a 96% sensitivity is available. None of the test methods is completely fail-safe nevertheless, except for the stomach lining biopsy in combination with urease test.
Treatment
One of the most important factors for treatment of H.Pylori induces gastric irritations is thin blood. The condition means there are too few platelets, a part of the blood that helps it clot. When your blood is thin, you will suffer from gastric irritation for longer period of time. The first step to naturally heal your gastric irritation is a good source of vitamin K2. Avoid vitamin K2 supplements. Simply eat the foods such as raw cabbage and romaine lettuce. This would help you heal the gastritis faster than with any other methods. You can also add a half spoon of baking soda with a 1/16th teaspoon of sodium chloride (non-iodized salt) on a full glass of water and use it as a mouth wash for 5-10 seconds for a few days to reduce body acidity and help healing the gastritis. Do NOT swallow the mixture.
The common mainstream medicine treatment typically consists of triple antibiotics regimen such as clarithromycin, metronidazole and amoxicillin. On the other hand, the success rate of total eradication is only about 40% since some strains (over 20) of H. Pylori are resistant to these antibiotics. Another co-factor is a partner reinfection after irradiation [srs] which may prompt additional round of antibiotic treatment resulting in further damage to a body. Therefore, it is recommended to treat all people in the household with herbal remedies rather than with drugs that have long term adverse effects on health.
Restoring the gastric acid production may play a significant role in reducing the overgrowth of H. Pylori.
The following alternative H. Pylori infection eradication protocol should be sustained for 2 months followed by retesting for the presence of infection about 3 months after the end of treatment.
The other best method to eradicate an infection is to start with bacterial growth inhibition. Mustic gum prevents the bacteria from attaching to stomach lining, and thus inhibits its replication. Other growth inhibitors are lactobacillus reuteri and Sulforaphane. Once the outgrowth is controlled with inhibitors, those agents that actually kill the bacteria could be used, such as monolaurin. Starting in the opposite order would produce significant die off side effects. Note that garlic, vinegar and digestive bitters actually kill the bacteria, and would produce a die off symptoms if started prematurely.
When proceeding with treatment, side effects of bacteria die-off released toxins are expected. These can include bloating, neurological symptoms, insomnia, restlessness and anxiety. If die off side effects are too intense and continue for more than a few days, reduce the amount of supplements and foods that kill the bacteria and gradually increase their amounts as the tolerance increases. Some individuals need to start with one dose once a week, and increase the frequency until tolerated.
| Supplements | Dietary adjustments |
Eradication Method 1
Eradication Method 2
Healing of the stomach lining inflammation (optional)
Other helpful supplements and factors (optional)
|
Avoid
Foods to consume (including glutathione boosting foods)
|
Once the bacteria is mostly eradicated and diet is normalized, it may take up to 6 months to feel significant improvements in health.
Following the treatment, mastic gum can be taken as a maintenance measure, since H. Pylori may become dormant and not completely eradicated. The maintenance dose of 500mg of mastic gum a few times a week is also indicated in prevention of reinfection from foods and partners. Reasonable dietary consumption of foods and herbs that help to suppress the growth of bacteria after the treatment is also helpful in prevention of H. Pylori recurrence.
Low stomach acid. Once the infection has been suppressed or even eradicated, the stomach acid production should start gradually restoring, however, it may remain below normal levels for some time. Using the stomach acid production supplements can help to normalize digestion and recover the normal function of parietal cells.